Main Page
A.A. Martinos Center / Wald group anthropomorphic phantom builder's Wiki
This Wiki is a resource for people interested in constructing anthropomorphic MRI phantoms developed by Larry Wald's group at the Martinos Center for Biomedical Imaging, Massachusetts General Hospital.
The basic principle is that improved anthropomorphic phantoms lead to better and faster development of MRI methodology with less use of healthy subject volunteers. This is both cost effective and ethical. Therefore we distribute our designs and ask only that you reference the appropriate paper and the source of the design.
Designs are available in standard CAD format are intended to be 3D printed. Most of the components are open source designs.
MGH Phantoms for download
Instructions for sealing, assembly and filing of 3D printed phantoms
This section contains general instructions for making 3D printed phantoms. More detailed/specific instructions are available for individual phantoms.
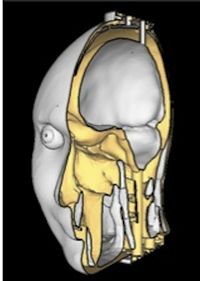
3D printing
Once you have downloaded the CAD files for a specific phantom, you should 3D print the different parts using your favorite 3D printer. Note that some parts may require you to be able to dissolve the support material, which is not always possible with all 3D printers (we have tried to add these 3D printing details for each phantom, but if you have any doubt contact Bastien Guerin [guerin at nmr dot mgh dot harvard dot edu]). This mostly affects complex parts such as the skull which has many grooves and cavities that may not be always easily reachable. If you do dissolve the support material using a solvent, make sure that the parts are clean and perfectly dry before continuing working with them (this may require leaving them in a well-ventilated area for one or two days).
When used for MRI, make sure that all parts are 3D printed as dense parts. Usually 3D printer offer the otpion to print a part either as "dense" or "sparse". The "sparse" option results in faster printing and lower consumption of plastic. However it is not adequate for MRI because the air trapped inside the small plastic cavities due to the sparse 3D printing option create off-resonance effects that may significantly distort images of the phantom. It is our experience that printing all plastic parts as "dense" is an absolute necessity at 7 Tesla. This problem may be less pronounced at lower field strength.
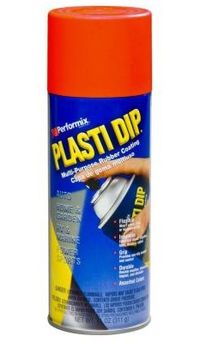
Waterproofing
The next step is to seal the parts. Even if your 3D printer offers a "waterproof" printing option, which is sometimes available on 3D printers, there is no guarantee that the parts will actually be waterproof. 3D printing of waterproof parts is actually very difficult. Most "waterproof" 3D printing strategies results in reasonably waterproof parts when these are flat (e.g., flat panels) but almost always fail for complex geometries such as a human head. Obviously, an MRI phantom should not leak since this would result in potential damage to the coil and other electronic components. We have experimented with several techniques including painting the plastic parts with epoxy and melting of the plastic surface with a solvent (acetone can be used to melt ABS parts. Methylene chloride can be used to melt polycarbonate plastic). We have found that these two methods do not work well however. The method that we currently use for all our models consists in spraying the parts with a rubber spray. For our phantoms, we apply three thick coats of rubber spray on the outside and the inside of all parts (covering the outside of the outer parts prevents leaks and sweating in the event where some water infiltrates the plastic parts because of failure of the inner-most rubber coat). We use a red rubber spray as opposed to a black one since the latter color is often achieved using ferrite nanoparticles that may be magnetic. Note that the parts must be entirely sealed with spray before assembly, including the small grooves and nudges (we impose a gap between fitting parts of at least 1 mm in our models in order to account for the increased thickness of the part due to the waterproof coating).
Assembly
Once all parts are waterproofed, simply assemble them by gluing them with epoxy. Apply a small pressure between the two parts during curing of the epoxy to ensure good sealing of the parts. If the phantom contains nested parts (e.g. a skull compartment inside an outer plastic shell), assemble the inner compartment first and then the outer one. Also, if the filling port of the inner compartment does not extend outside the phantom do not forget to fill the compartment before assembling the outer compartment!
Filling
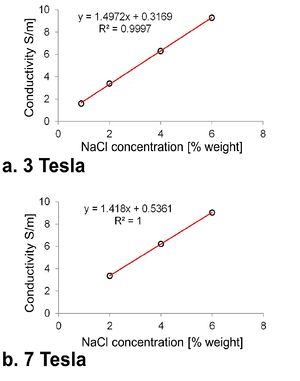
The final step consists in filling the various compartments with some kind of gel. We use the following mixture to mimic human tissues (all concentrations are in percent of the total weight):
- Agar: 1% to 3% depending on the desired viscosity. When mixed with water, a 1% agar solution has a tick but liquid consistency. A water-based 3% agar solution is solid at room temperature. - Gadolinium: 0.1%, this is useful to reduce T1 and hence allows faster testing of protocols by reduction of TR. - Salt (NaCl): This is required for increasing the conductivity of the mixture and hence loading of the coil. See the graph on the right to determine the appropriate concentration. - Sodium Azide (NaN3): 0.05%, this is used to prevent bacterial growth.
Additionally, one can add ethylene glycol in powder form to obtain a more realistic permittivity (the mixture above has a permittivity close to that of water, ~80, which is greater than the permittivity of biological tissues, ~50). You can experiment with that if you have a dielectric probe, however the concentrations of ethylene glycol required to significantly lower the permittivity are large which may change other parameters of the mixture such as its consistency and its conductivity. In order to prepare the mixture, we recommend the following step-by-step process:
- Heat the water in glass containers using a microwave until the water boils. - Add all the ingredients except the agar and mix well. - If you kept the water hot using a hot plate, turn it off (otherwise you will burn the agar at the bottom of the container). Slowly pour the agar powder in the hot mixture while stirring continuously to avoid the formation of large lumps of undissolved agar. Note that for the agar to dissolve well, the water temperature should be at least 80 degrees Celsius.
Before filling the phantom you may want to wait an hour or two so that the mixture cools a bit and doesn't damage the waterproof rubber coating. Also keep in mind that agar shrinks in volume as it cools down, therefore the compartment may not be completely filled. To deal with this, you can fill the compartment, then wait overnight for the mixture to cool down and the next day add some of the leftover mixture to completely fill the compartment. You can then seal the compartment using hot glue.
References
[http://www.ncbi.nlm.nih.gov/pubmed/17659546 Design, Construction and Evaluation of an Anthropomorphic Head Phantom With Realistic Susceptibility Artifacts
[http://www.ncbi.nlm.nih.gov/pubmed/3821466 New Polyvinyl Alcohol Gel Material for MRI Phantoms
[http://www.ncbi.nlm.nih.gov/pubmed/16148391 Tissue-mimicking phantom materials for narrowband and ultrawideband microwave applications
[http://www.ncbi.nlm.nih.gov/pubmed/22396226 A Novel MRI-Compatible Brain Ventricle Phantom for Validation of Segmentation and Volumetry Methods
[http://www.ncbi.nlm.nih.gov/pubmed/21866208 Heterogeneous Anthropomorphic Phantoms With Realistic Dielectric Properties For Microwave Breast Imaging Experiments
[http://www.ncbi.nlm.nih.gov/pubmed/22225325 An anthropomorphic polyvinyl alcohol brain phantom based on Colin27 for use in multimodal imaging